HYADENT BG
Description:
The natural promoter of regeneration
Hyaluronic Acid
HA Gel composed of a mixture of cross-linked (1,6%) and natural (0,2%) Hyaluronic Acid
2 x 1.2 ml cylindrical ampulla
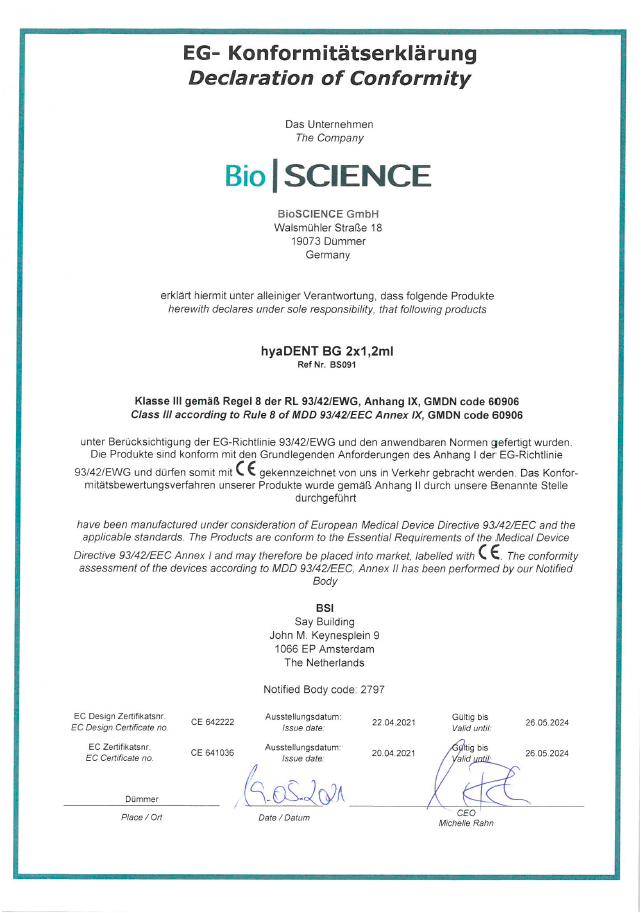
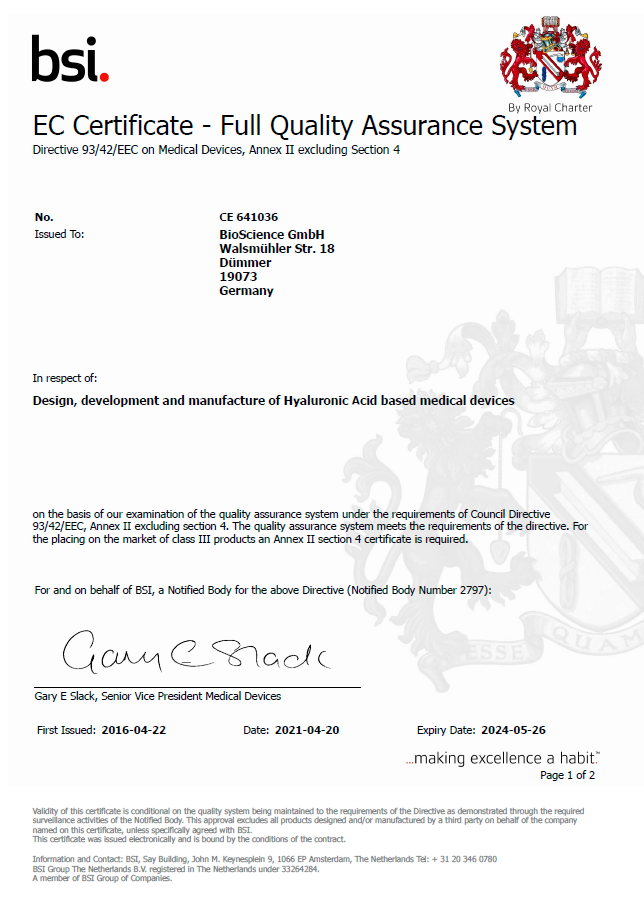
Certificates, instructions
 Delivery
Is free of charge within 24 hours after funds are credited to your Bank account
Delivery
Is free of charge within 24 hours after funds are credited to your Bank account
Files, documents
Clinical cases
Description
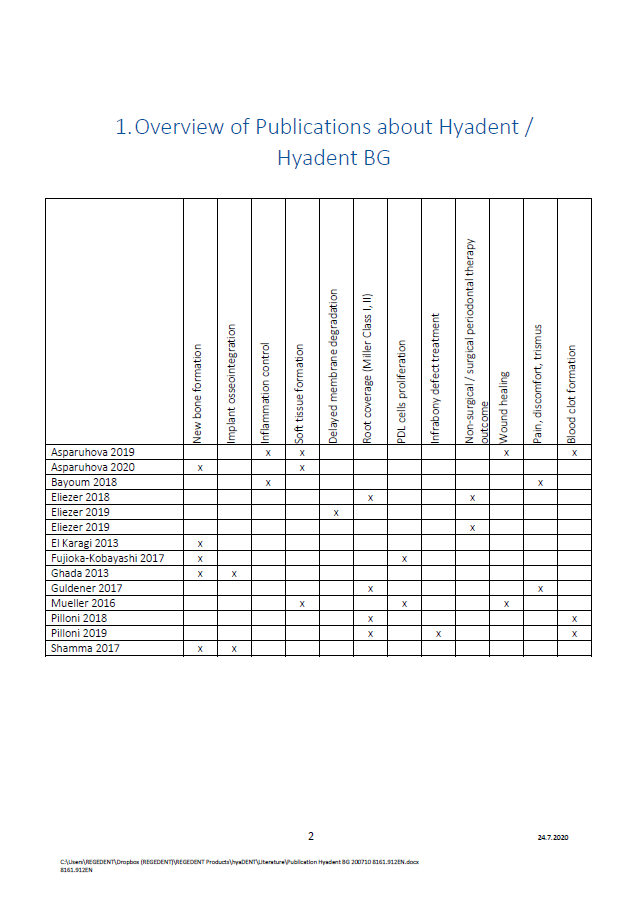
What shows that xHya (cross-linked hyaluronic acid) helps Guided Bone Regeneration?

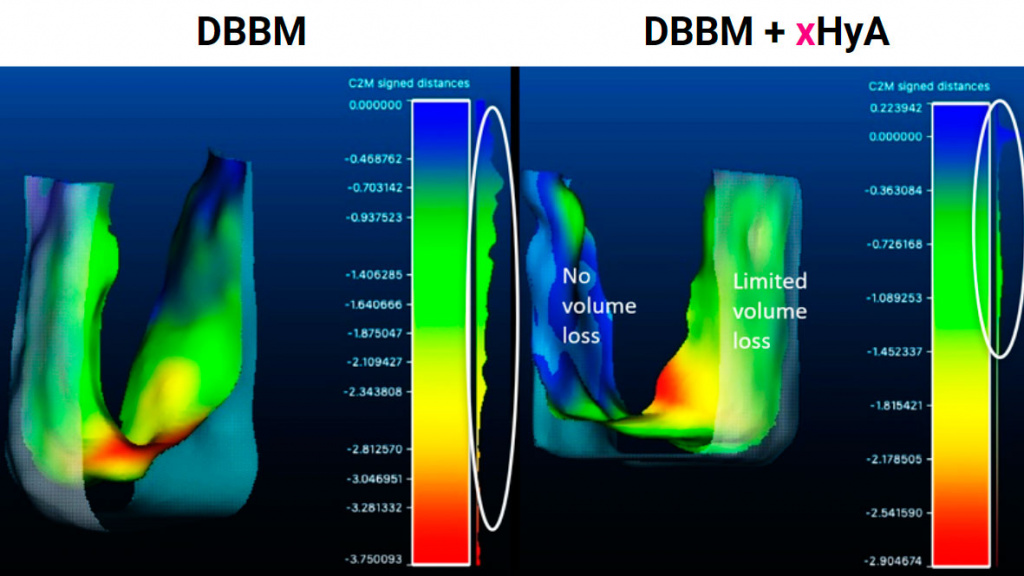
Better volume stability after 6 months with DBBM + xHyA
Mandibular median width (mm)
Kauffmann et al. (submitted)
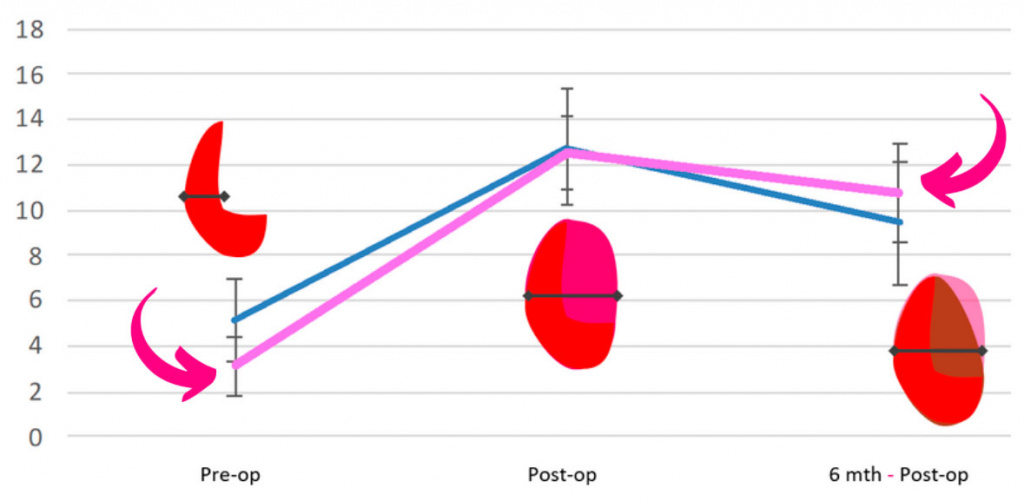
Better volume stability after 2 months with DBBM + xHyA
Mandibular median width (mm)
Split mouth case of ridge preservationi
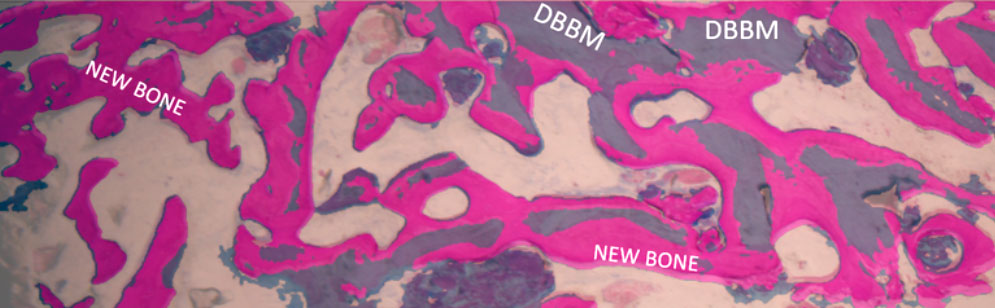
More bone cells, better DBBM remodelling, limited soft-tissue growth after 2 months with DBBM + xHyA
DBBM:
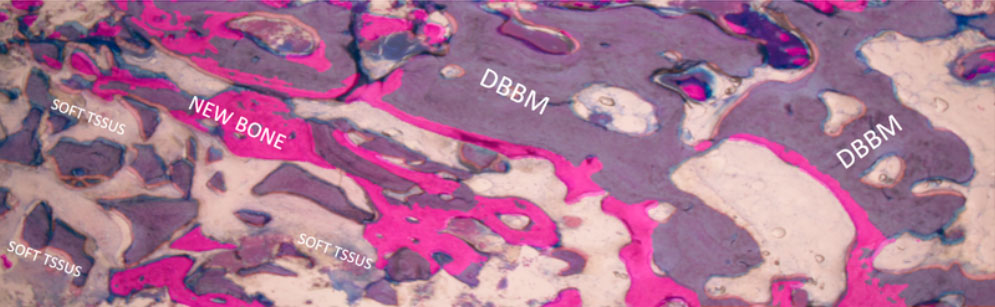
DBBM + xHyA:
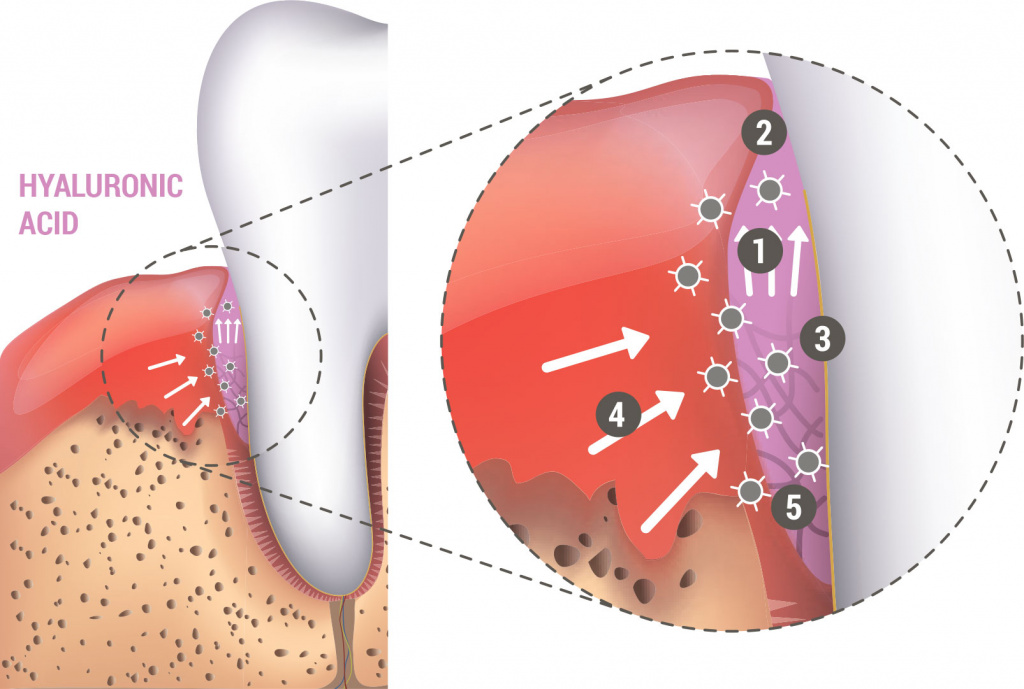
HYALURONIC ACID-EFFECTS

HYADENT BG, a highly concentrated and cross-linked hyaluronic acid gel, is designed specifically for the application in the dental field
Hyaluronic acid (HA), as one of main components of the extracellular matrix is naturally present in the human body1-3. Studies have shown that prolonged presence of HA during the healing process promotes healing by regeneration rather than reparation4,5.
Besides accelerating the healing of soft tissue and bone6,7,8, the bacteriostatic properties of HA also protect the wound9.
HYADENT BG remains present throughout the various phases of the healing process due to its slow degradation pattern (several weeks)10.
In addition, it aids the surgical periodontal treatment after application to the root surface and soft tissue.
This leads to faster wound closure, substantial pocket reduction and enhanced attachment11-13. When mixed with bone substitute material of any origin HYADENT BG forms an easily manageable putty, which may in addition lead to accelerated bone formation.14,15.
HYADENT BG is a hyaluronic acid-based treatment solution of non- animal origin optimized for regenerative dental and periodontal applications.
- Accelerated tissue healing
Coordinates the post-operative inflammation process and accelerates angiogenesis11,16,17 - Improved outcome
Stabilizes coagulum and supports tissue regeneration11-13,16 - Improved predictability
Bacteriostatic action and reduced pathogen penetration9
Principle of operation
- Attracts blood
- Stabilizes coagulum and supports tissue regeneration
- Bacteriostatic effect provides protection
- Growth factors attracted by hyaluronic acid
- Coordinates inflammation and accelerates angiogenesis
Video
References
- Lee JY, Spicer AP. ‘Hyaluronan: a multifunctional, megadalton, stealth molecule.’ Curr Opin Cell Biol 2000;12:581–586.
- McDonald J, Hascall VC. ‘Hyaluronan mini review series.’ JBiol Chem 2002; 277:4575–4579.
- Jiang D et al. ‘Hyaluronan as an immune regulator in human diseases.’ Physiol Rev 2011;91:221–264.
- Longaker T et al. ‘Studies in Fetal Wound Healing: V. A prolonged presence of hyaluronic acid characterizes fetal wound healing’ Ann. Surg. 1991; April:292–296.
- Mast BA et al. ‘Hyaluronic Acid Modulates Proliferation, Collagen and Protein Synthesis of Cultured Fetal Fibroblast’ Matrix, 1993;13:441–446
- Salbach J et al. ‘Regenerative potential of glycosaminoglycans for skin and bone.’ J Mol Med 2012;90:625–635.
- Muzaffer A. et al. ‘The Effect of Hyaluronic Acid-supplemented Bone Graft in Bone Healing: Experimental Study in Rabbits ’ J Biomater Appl 2006 20:209
- Sasaki T, Watanabe C, Bone. Vol. 16. No.1 January 1995:9-15
- Pirnazar P. et al. ’Bacteriostatic effects of hyaluronic acid.’ Journal of Periodontology 1999;70:370-374
- De Boulle K, Glogau R, Kono T, et al. ‚A Review of the Metabolism of 1,4-Butanediol Diglycidyl Ether– Crosslinked Hyaluronic Acid Dermal Fillers.’ Dermatologic Surgery 2013;39(12):1758-1766
- King SR, Hickerson WL, Proctor KG. Benefi cial actions of exogenous hyaluronic acid on healing. Surgery 1991;109(1):76-84
- Fawzy ES. et al. Local application of hyaluronan gel in conjunction with periodontal surgery: a randomized controlled trial. Clin Oral Invest 2012;16:1229-1236
- Briguglio, F. et al. Treatment of infrabony periodontal defects using a resorbable biopolymer of hyaluronic acid: A randomized clinical trial. Quintessence Int 2013;44:231-240
- Stiller M. et al. ‘Performance of β-tricalcium phosphate granules and putty, bone grafting materials after bilateral sinus fl oor augmentation in humans’ Biomaterials 2014;35(10):3154-3163.
- Mendes RM et al. ‘Sodium hyaluronate accelerates the healing process in tooth sockets of rat’ Arch Oral Biol 2008; 53:1155–1162
- Kessiena L. Aya et al. ‘Hyaluronan in wound healing: Rediscovering a major player.’ Wound Rep Reg 2014;22:579-593. Dental Journal. (2017) Vol.42:104-11.
- West DC et al. ‘Angiogenesis induced by degradation products of hyaluronic acid.’ Science. 1985 Jun 14;228(4705):1324-6.
| Other | ||
| Клинические случаи БЗ | Periodontal regeneration in deep infrabony defects with CaP/ß-TCP and hyaluronic acid / Coverage of Miller class 3 (RT2 Class A+) recession with CTG + HA using modified Tunneling technique | |
| KEYWORDS RU | hyadent bg, регенерация тканей | |
 Delivery
Is free of charge within 24 hours after funds are credited to your Bank account
Delivery
Is free of charge within 24 hours after funds are credited to your Bank account





 Catalog
Catalog 






























 Subscribe
Subscribe Buy in 1 click
Buy in 1 click Out of stock
Out of stock